Overview
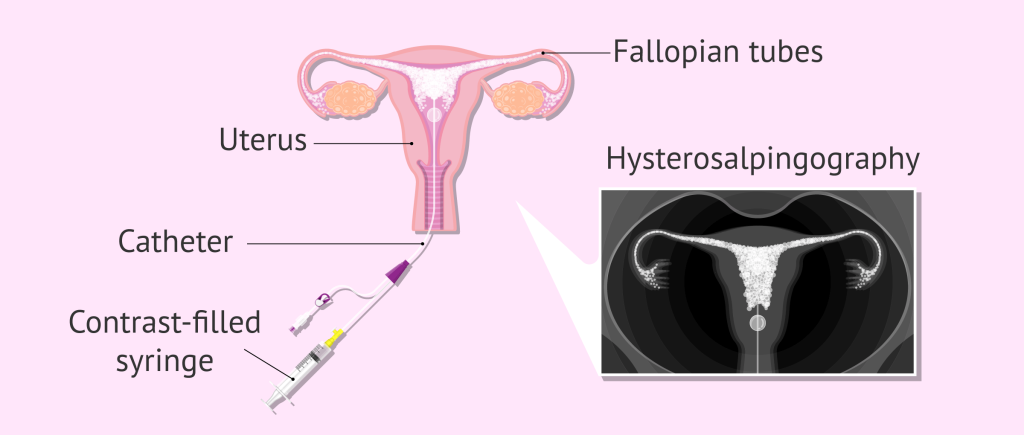
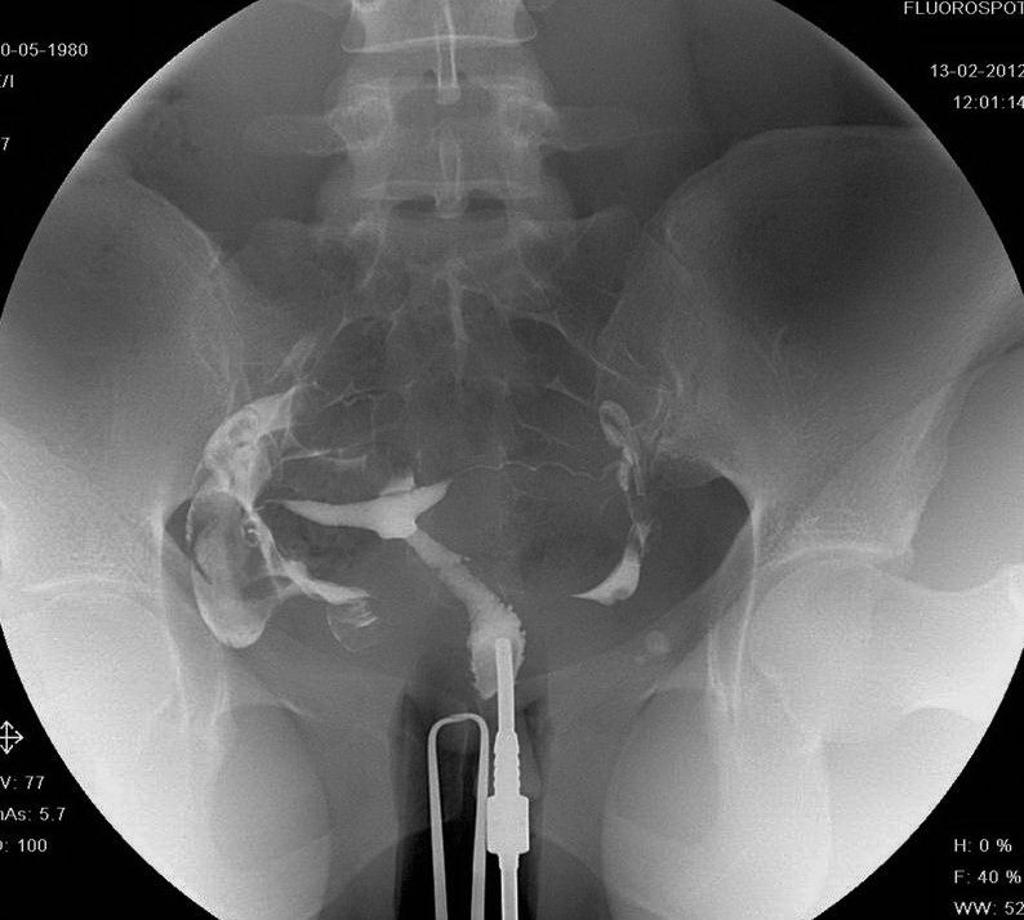
Hysterosalpingography (HSG) is a diagnostic procedure that is used to assess the health of a woman’s uterus and fallopian tubes. It is done to evaluate any structural issues that could be contributing to infertility or repeated miscarriages. Women who have trouble getting pregnant or who frequently miscarry are typically advised to have the procedure.
CONDITIONS DIAGNOSED By HSG
The following are a few of the most typical conditions that can be identified with HSG:
- Blockages in the fallopian tubes: HSG can aid in locating any obstructions or blockages in the fallopian tubes that may prevent the egg from making it to the uterus in time for fertilization. Conditions including pelvic inflammatory illness, endometriosis, or prior surgery can all result in blockages.
- Uterine abnormalities: HSG can also be used to find uterine polyps, fibroids, and other congenital or acquired uterine deformities. Infertility or repeated miscarriages may result from these disorders.
- Adhesions: HSG can also detect the existence of adhesions, which are abnormal tissue bands that can develop inside the pelvic cavity and are frequently brought on by endometriosis, surgery, or infection. Adhesions may result in infertility or discomfort during sexual activity.
- Scarring: HSG can also identify whether the uterus or fallopian tubes have been scarred. Conditions like Asherman’s syndrome, which results in the production of scar tissue in the uterus, can lead to scarring.
- Ectopic Pregnancy: An ectopic pregnancy is one that develops outside the uterus, typically in the fallopian tube, and HSG can help detect it. Ectopic pregnancy is a medical emergency that needs to be treated right away.
PROCEDURE
Here is a thorough explanation of the HSG process:
- Pre-operation instructions: The patient will be instructed to fast for a number of hours prior to the surgery. The patient may also receive a light sedative to aid in relaxation. Before the treatment, the patient should make the doctor aware of any allergies or other medical issues.
- Cervical dilation: The process starts with the patient reclining on a table in a stirrup posture. The cervix will be dilated (widened) with a dilator, and a speculum will be inserted to hold it open.
- Injection of contrast material: After the cervix has been widened, a small, flexible tube will be put through it and into the uterus. The contrast agent (dye) is then delivered into the uterus through the tube.
- X-ray imaging: Pictures of the uterus and fallopian tubes will be taken when the contrast material passes through them. The uterus and fallopian tubes can be seen by the radiologist, and any obstructions or abnormalities can be seen on the X-ray.
- Length of the procedure: The whole thing usually takes 15 to 20 minutes, during which the patient may feel cramps or pain.
- Post-operative instructions: The patient can return home and carry on with their regular activities following the surgery. After the surgery, the patient can have some cramping or spotting for a few days. To help the body flush the contrast material out, it’s necessary to drink enough water.
- Results: A radiologist will review the X-ray images and search for any anomalies or obstructions in the fallopian tubes or uterus. If any are discovered, additional examinations or medical care may be suggested.
Other Service
Need help ?
Expertise and advanced technology are both essential for better diagnosis of the body. Contact us if you require any assistance with your diagnostics.